THE ORAL SYSTEMIC CONNECTION
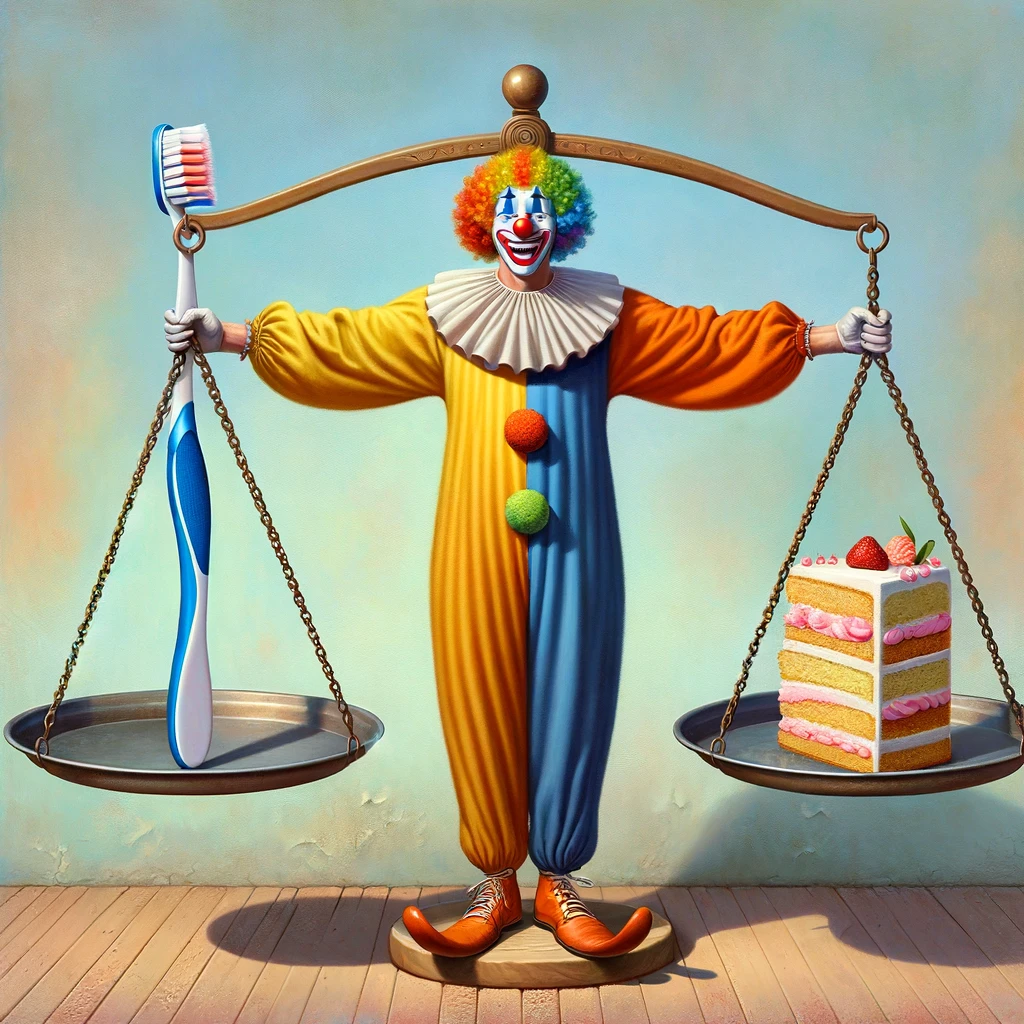
As a diabetic, you’re no stranger to the careful balancing act of managing your health. But did you know there’s a crucial piece of the puzzle that often goes unnoticed? It’s your oral health, specifically periodontal (gum) disease, a condition that quietly walks hand in hand with diabetes.
The relationship between periodontal disease and diabetes, rheumatoid arthritis and cardiovascular disease is well established. Evidence suggests that this bi-direction interaction impacts progression, severity, and mortality. This isn’t just about oral health; it’s about your lifespan, your moments with loved ones and your memories yet to be made.
Don’t let periodontal disease shorten your story. A brighter future and a longer life are within reach, starting with the health of your gums. But first, you have to know what condition your gums are in.
That’s where we can help. Call us to schedule an Advanced Oral Evaluation Exam™. Discover the true state of your gum health and take a decisive step toward not just managing your diabetes but thriving despite it. Your journey to a healthier, longer life is just a phone call away. Don’t wait for tomorrow; take control today.